Two men from Texas and Florida were sentenced today to four years and two years in prison, respectively, for their roles as leaders of a marketing company that solicited Medicare beneficiaries for medically unnecessary genetic testing. The Florida man received an additional two years in prison, to be served concurrently, for his role in falsifying the ownership information in Medicare enrollment documentation for a clinical laboratory.
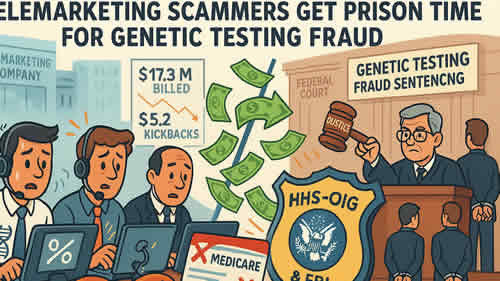
According to court documents, Paul Wexler, 56, of Spring, Texas, and Paul Bleignier, 64, of Seminole, Florida, operated a telemarketing company that recruited Medicare beneficiaries for cancer genetic (CGx) testing that was medically unnecessary. CGx testing uses DNA sequencing to detect mutations in genes that could indicate a higher risk of developing certain types of cancers in the future. It is not a method of diagnosing whether an individual presently has cancer, and Medicare covers CGx testing in limited circumstances. Further, Wexler, Bleignier and their co-conspirators solicited and received kickbacks in exchange for referring Medicare beneficiaries for CGx testing that was not eligible for Medicare reimbursement. Through the scheme, Wexler and Bleignier caused Medicare to be billed $17.3 million, and they were paid $5.2 million.
While the criminal case for genetic testing fraud was pending, Bleignier opened a clinical laboratory and enrolled it in Medicare. Medicare requires a certification listing anyone with 5% or more ownership interest, but Bleignier used other people’s identities to disguise his involvement. The claims related to that laboratory were further tainted by kickbacks. Bleignier and his co-conspirators billed Medicare for $3,012,156 in claims that were ineligible for reimbursement, and they were paid $916,106.
In April 2024, Wexler pleaded guilty to conspiracy to commit health care fraud and wire fraud. In November 2022, Bleignier pleaded guilty to conspiracy to defraud the United States and pay and receive kickbacks, and in November 2024, he pleaded guilty to making false statements related to health care matters. At sentencing the two were ordered to pay $1.2 million in forfeiture each and $5.2 million in restitution. Bleignier was ordered to pay an additional $916,106 in forfeiture for his role in falsifying the ownership information in Medicare enrollment documentation.
Acting Assistant Attorney General Matthew R. Galeotti of the Justice Department’s Criminal Division; U.S. Attorney Gregory W. Kehoe for the Middle District of Florida; and Deputy Inspector General for Investigations Christian J. Schrank of the U.S. Department of Health and Human Services, Office of Inspector General (HHS-OIG) made the announcement.
HHS-OIG and FBI investigated the case.
Trial Attorney Charles D. Strauss of the Criminal Division’s Fraud Section prosecuted the case.
The Fraud Section leads the Criminal Division’s efforts to combat health care fraud through the Health Care Fraud Strike Force Program. Since March 2007, this program, currently comprised of nine strike forces operating in 27 federal districts, has charged more than 5,800 defendants who collectively have billed federal health care programs and private insurers more than $30 billion. In addition, the Centers for Medicare & Medicaid Services, working in conjunction with the Office of the Inspector General for the Department of Health and Human Services, are taking steps to hold providers accountable for their involvement in health care fraud schemes. More information can be found at www.justice.gov/criminal-fraud/health-care-fraud-unit.
Updated November 13, 2025
Office of Public Affairs
Sources: Justice.gov , Midtown Tribune News
